What to do about shin splints:
Part 1:
The Diagnosis
~
Part 1: The Diagnosis ~
In high school I was a field athlete- a pole vaulter to be exact (don’t get excited, I was terrible at it). I have this very distinct memory of my shins starting to hurt. “It’s shin splints”, my enlightened track friends told me. “You gotta put tape on your shin like mine and do duck walks”, they advised.
Sounded reasonable. On the way to practice the next day, I popped into the training room to grab the white roll of athletic tape. I distinctly remember the Athletic Trainer being irate with me for jumping into treating myself without being evaluated by her. Having no idea what an ATC actually was, nor thinking that I would benefit from her expert supervision (ah, teenagers…) I ignored her, grabbed the tape, and headed out the door.
Ultimately, my shin splints worked themselves out, probably because I didn’t really train that hard. (That may explain my horrible performance at track meets, but I digress). Nonetheless, the memory has lingered with me over the years as I became a runner and endurance athlete. It pops up every time I see someone self-diagnose their shin splints. I chew on the diagnosis as one dines on white bread- it feels like it’s doing the job yet somehow doesn’t seem to hold enough substance to be satisfying.
Shin splints isn’t necessarily a wrong diagnosis. My concern is that it has become a garbage term used to describe shin pain without ever giving the patient an opportunity to reach a more definitive explanation of the cause and treatment.
This article will be divided into three parts:
Describe Shin splints: What is it really? How is it different from other shin pain?
Assessing Lower Leg Dysfunctions: We’re going to explore the biomechanical drivers behind shin splints. You’ll learn a super simple screen to help you understand your own lower leg risk factors.
Self-care: We’ll lay out the path to recovery.
PART 1
What are shin splints?
As mentioned before, the term “shin splints” is thrown around quite a lot to describe any pain within the middle lower leg region. Medically, the term refers to “medial tibial stress syndrome”. All this means is that there is pain along the medial side of your tibia (the big shin bone), usually somewhere in the bottom third, as a result of repetitive load to the musculotendinous attachments. If you’ve ever described a pain along the lateral side of your tibia as shin splints, you wouldn’t be incorrect, this would be considered “anterior tibial stress syndrome”
There are two theories behind shin splints:
Traction Theory- The muscles attached to the tibia are put under repetitive strain, causing wear and tear that leads to inflammation. The primary victims/culprits: Tibialis Posterior, Soleus, Flexor Digitorum Longus, Deep fascia.
“Bone Stress-Failure”- The tibia has an inadequate response to repetitive forces, either driven by poor biomechanics, muscular imbalances, or weakness within the bony matrix.
Both of these theories point to one underlying theme: The tissues of the lower leg are being placed under repetitive stress that they are unable to withstand.
What else can it be?
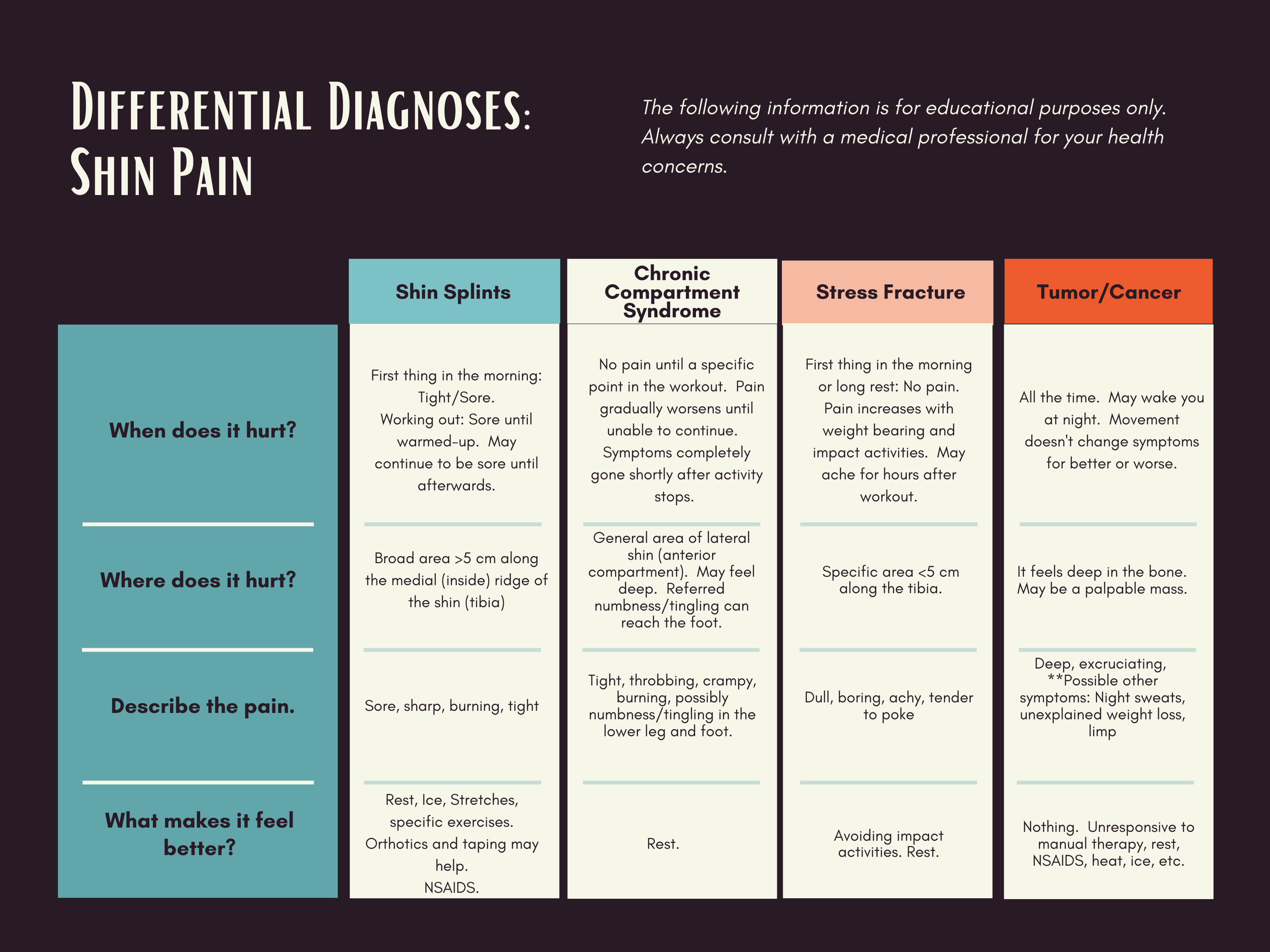
Shin splints must be distinguished from other potential problems. This can take a long time to parse out, especially if you are self-diagnosing. This is why it is critical to understand your symptoms and to work with a pro for assessment and treatment. When considering shin pain, the 4 primary diagnosis considered are: Medial Tibial Stress Syndrome, Chronic Compartment Syndrome, Stress Fractures, and (big outlier) tumors/cancer.
As you can see from the chart, the biggest questions are: When does the pain start, stop, and what does it feel like? True shin splints are driven by exercise, often paired with sensations of muscular pain (tight, sore, etc). An important consideration is that shin splints are a risk factor for stress fractures.
I’ll share an unforgettable moment at my senior year regional track meet. An athlete from a competing school was racing against my friends in a distance event. Suddenly she collapsed, sobbing; my friends later whispered that they heard loud POPs just before she went down. Rumor had it that this young woman was determined to make it to States and earn a 4.0 GPA; she had spent the entire year self-treating her shin splints with ibuprofen. Instead, she had placed so much stress on her legs that the tibias- both of them- fractured mid-run. This young woman recovered and continued to run in college (I know because we landed in the same college where I worked as a student athletic trainer); but she carried scars on her shins as a testimony to the complicated recovery she endured.
All that to say…
It is important to recognize the when and what of your shin pain. In Part 2, we will look at movement assessments and how your squat can reveal risk factors for injury.